- 1. 🌱 Why 35 Is Considered a Fertility Milestone
- 2. 🧠 What Actually Changes When Trying to Conceive After 35
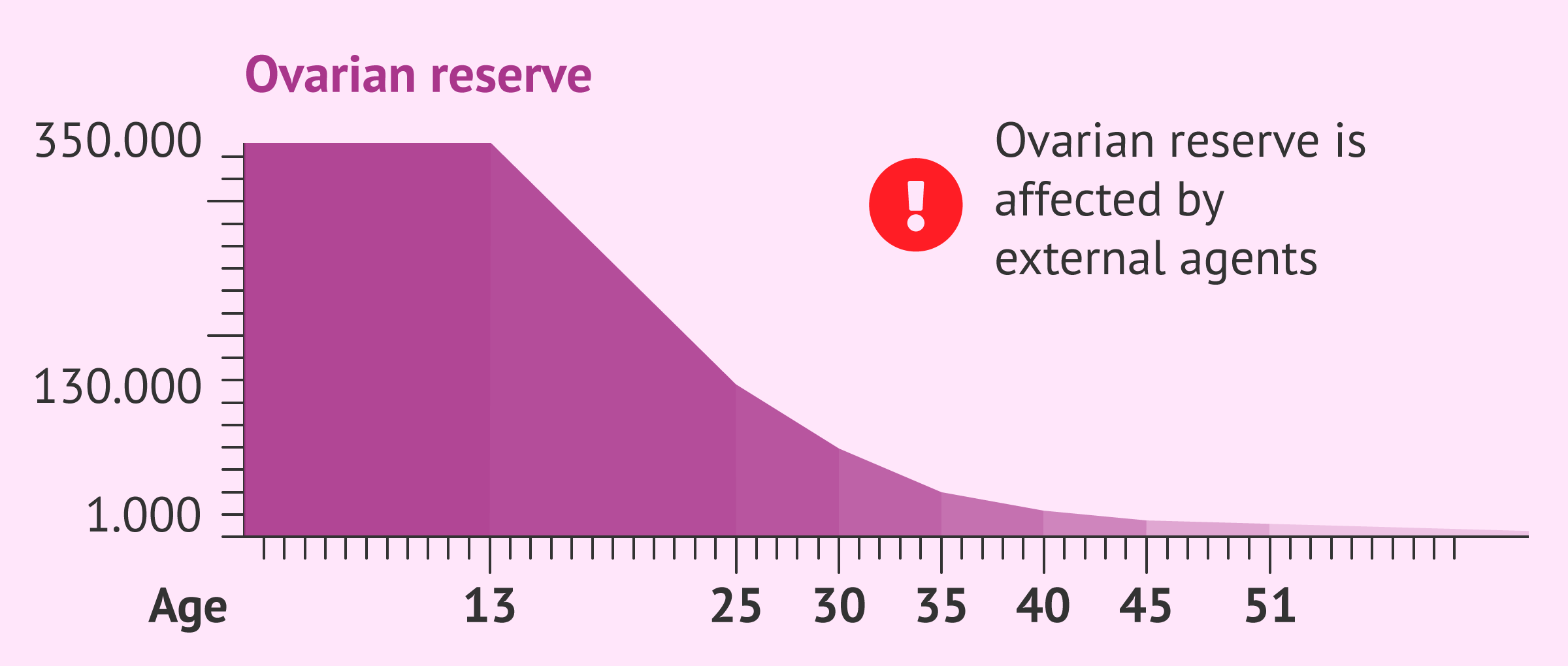
- 2.1. 1️⃣ Egg Quantity (Ovarian Reserve) Declines
- 2.2. 2️⃣ Egg Quality Becomes More Important
- 2.3. 3️⃣ Time to Pregnancy May Increase
- 2.4. 4️⃣ Miscarriage Risk Increases (But Is Still Not the Norm)
- 2.5. 5️⃣ Hormone Balance May Be Less Predictable
- 3. 🚫 Common Myths About Trying to Conceive After 35
- 3.1. ❌ Myth: “It’s too late”
- 3.2. ❌ Myth: “You’ll definitely need IVF”
- 3.3. ❌ Myth: “Every month wasted is catastrophic”
- 4. 🌿 How to Improve Your Chances When TTC After 35
- 4.1. 1️⃣ Track Ovulation More Intentionally
- 4.2. 2️⃣ Focus on Egg Quality Support
- 4.3. 3️⃣ Start Supplements Earlier (and Smarter)
- 4.4. 4️⃣ Don’t Ignore Male Fertility
- 4.5. 5️⃣ Manage Stress Without Blaming Yourself
- 5. 🧪 When to Seek Medical Support After 35
- 6. ⏳ A Realistic TTC Timeline After 35
- 7. 💛 Emotional Side of TTC After 35
- 8. 🔗 Internal Links (Cluster Support)
- 9. 🧠 Final Thoughts

Trying To Conceive After 35 What Changes How To Improve Your Chances Fertiease
Trying to conceive after 35 can feel intimidating. You may hear phrases like “advanced maternal age” or “time is running out,” which can create unnecessary fear. While it’s true that fertility changes with age, many women successfully conceive and have healthy pregnancies after 35.
The key is understanding what actually changes, what doesn’t, and how to support your body intelligently during this stage.
In this evidence-based guide, we’ll explain what happens to fertility after 35, common myths, realistic timelines, and practical steps to improve your chances of conceiving.
🌱 Why 35 Is Considered a Fertility Milestone
The age of 35 is often highlighted because:
Egg quantity begins to decline more noticeably
Egg quality gradually decreases
Chromosomal abnormalities become more common
Time to conception may increase
However, 35 is not a fertility cliff. It’s a transition point—not a deadline.
🧠 What Actually Changes When Trying to Conceive After 35
1️⃣ Egg Quantity (Ovarian Reserve) Declines
Women are born with all the eggs they’ll ever have. Over time:
The number of remaining eggs decreases
Fewer eggs respond to ovulation signals
This doesn’t mean you can’t conceive—it may just take longer.
2️⃣ Egg Quality Becomes More Important
After 35:
Eggs are more likely to have chromosomal errors
This can affect fertilization or implantation
Egg quality—not just quantity—is often the main factor.
3️⃣ Time to Pregnancy May Increase
Younger couples may conceive within 3–6 months.
After 35:
It may take closer to 6–12 months
This is still considered normal
Patience and consistency matter more than urgency.
4️⃣ Miscarriage Risk Increases (But Is Still Not the Norm)
Miscarriage risk does rise with age due to chromosomal issues.
However:
Most pregnancies after 35 do not end in miscarriage
Many women go on to have healthy babies
Statistics describe populations—not individual outcomes.
5️⃣ Hormone Balance May Be Less Predictable
After 35, you may notice:
Shorter cycles
Changes in luteal phase length
More pronounced PMS
These don’t automatically mean infertility—but they may require more awareness.
🚫 Common Myths About Trying to Conceive After 35
❌ Myth: “It’s too late”
Reality: Many women conceive naturally at 35–40+.
❌ Myth: “You’ll definitely need IVF”
Reality: Most women after 35 still conceive without assisted reproduction.
❌ Myth: “Every month wasted is catastrophic”
Reality: Smart preparation matters more than panic.
📌 Related read:
👉 Fertility Myths vs Reality (Evidence-Based)
🌿 How to Improve Your Chances When TTC After 35
1️⃣ Track Ovulation More Intentionally
Because cycles may be less predictable:
Use ovulation predictor kits (OPKs)
Track basal body temperature (BBT)
Watch cervical mucus patterns
Understanding your fertile window is crucial.
2️⃣ Focus on Egg Quality Support
Egg quality can’t be reversed—but it can be supported.
Helpful strategies include:
Antioxidant-rich foods
Omega-3 fatty acids
Adequate sleep
Stress reduction
📌 Related reads:
👉 Foods That Support Fertility Naturally
👉 Vitamins to Help Conceive
3️⃣ Start Supplements Earlier (and Smarter)
Women TTC after 35 often benefit from:
Prenatal vitamin with methylated folate
Vitamin D (if deficient)
Omega-3 (DHA + EPA)
CoQ10 (commonly recommended for 35+)
📌 Related read:
👉 How Long Should You Take Supplements Before TTC?
4️⃣ Don’t Ignore Male Fertility
Sperm quality declines with age too.
If your partner is 35+:
Male fertility supplements may help
Nutrition, sleep, and stress management matter
📌 Related read:
👉 TTC Supplements for Men
5️⃣ Manage Stress Without Blaming Yourself
Stress doesn’t “cause” infertility—but chronic stress can:
Disrupt ovulation
Affect hormone balance
Lower libido and consistency
Choose stress reduction methods that feel supportive—not forced.
🧪 When to Seek Medical Support After 35
Medical guidelines recommend:
Seeking evaluation after 6 months of trying if over 35
Earlier if cycles are irregular or absent
This isn’t a failure—it’s a proactive step.
Tests may include:
Hormone panels (FSH, AMH, TSH)
Ultrasound for ovarian reserve
Semen analysis for partner
Early insight saves time.
⏳ A Realistic TTC Timeline After 35
| Time Trying | What’s Normal |
|---|---|
| 0–3 months | Learning your cycle |
| 3–6 months | Many conceive here |
| 6 months | Reasonable point to seek guidance |
| 6–12 months | Still normal for many |
| 12+ months | More targeted support helpful |
You are not behind—you’re informed.
💛 Emotional Side of TTC After 35
Trying to conceive later can bring:
Pressure
Comparison
Fear of running out of time
These feelings are valid—but they don’t define your outcome.
Support matters:
Open communication with your partner
Trusted medical guidance
Compassion for yourself
🔗 Internal Links (Cluster Support)
👉 Coming Off Birth Control: How Long Until Fertility Returns?
👉 Best Fertility Supplements
👉 Foods That Support Fertility Naturally
👉 Fertility Myths vs Reality
🧠 Final Thoughts
Trying to conceive after 35 isn’t about panic—it’s about informed preparation.
Yes, fertility changes with age.
But knowledge, nutrition, timing, and support can significantly improve your chances.
35 is not the end of fertility.
It’s the beginning of a more intentional journey.
Your body is still capable.
Your options are still wide.
And your story is still being written.
What is your reaction to this article?
Here is a professional English bio for Dr. Elizabeth Williams, Obstetrician-Gynecologist: Dr. Elizabeth Williams, MD, FACOG, is a board-certified obstetrician-gynecologist with over 15 years of experience providing compassionate, evidence-based women’s healthcare. She earned her medical degree from Johns Hopkins University School of Medicine and completed her residency in Obstetrics and Gynecology at Massachusetts General Hospital, Harvard Medical School, where she served as Chief Resident. Dr. Williams specializes in high-risk pregnancies, minimally invasive gynecologic surgery, adolescent gynecology, and menopause management. Known for her warm bedside manner and clear communication, she is dedicated to empowering her patients through every stage of life, from prenatal care and childbirth to preventive wellness and complex gynecologic conditions. In addition to her clinical practice, Dr. Williams is actively involved in medical education and has published research on preeclampsia, labor induction, and robotic-assisted surgery. She is a Fellow of the American College of Obstetricians and Gynecologists (FACOG) and a member of the Society for Maternal-Fetal Medicine. Patients describe Dr. Williams as “attentive, knowledgeable, and truly caring,” and she is proud to deliver hundreds of babies each year while building long-term relationships with the families she serves. Dr. Williams practices in [City/State] and is affiliated with [Hospital Name]. She welcomes new patients and offers both in-person and telemedicine appointments.
VIEW AUTHOR PROFILE