- 1. 🌱 Why Early Pregnancy Exercise Matters
- 2. ⚠️ First Trimester Reality Check
- 3. 🤰 What’s Safe in Early Pregnancy Exercise?
- 3.1. Safe & Beneficial Activities
- 4. ❌ What’s NOT Safe in Early Pregnancy Exercise?
- 4.1. Avoid or Modify:
- 5. 💛 The Most Important Rule: Listen to Your Body
- 6. 💪 Early Pregnancy Exercise: 9 Powerful Tips for the First 12 Weeks
- 6.1. 1. Prioritize Breathing First
- 6.2. 2. Move in Short Sessions
- 6.3. 3. Keep Intensity Moderate
- 6.4. 4. Use Hydration Strategically
- 6.5. 5. Don’t Train to “Burn Calories”
- 6.6. 6. Avoid Breath Holding
- 6.7. 7. Track Energy Instead of Numbers
- 6.8. 8. Protect Your Core Early
- 6.9. 9. Rest Without Guilt
- 7. 🌼 Early Pregnancy Exercise by Trimester Progression
- 8. 🧬 When to Stop and Get Medical Guidance
- 9. 📌 Internal Links for Cluster Support
- 10. ✅ Final Thoughts
The first trimester is an emotional rollercoaster. You’ve just found out you’re pregnant—or you’re waiting to confirm—and suddenly everything feels like a risk. One of the biggest concerns women have is whether early pregnancy exercise is safe in the first 12 weeks.
Between old beliefs (“just rest, don’t move too much”) and new advice (“stay active!”), confusion is normal. But here’s the truth: for most women, staying active during early pregnancy is safe, beneficial, and encouraged—as long as you follow the right guidelines.
In this expert-backed guide, you’ll learn why exercise matters in early pregnancy, what’s safe, what to avoid, and 9 powerful tips that support your body during the most delicate stage of pregnancy.
Early Pregnancy Exercise Whats Safe In The First 12 Weeks 9 Powerful Tips 2 Fertiease
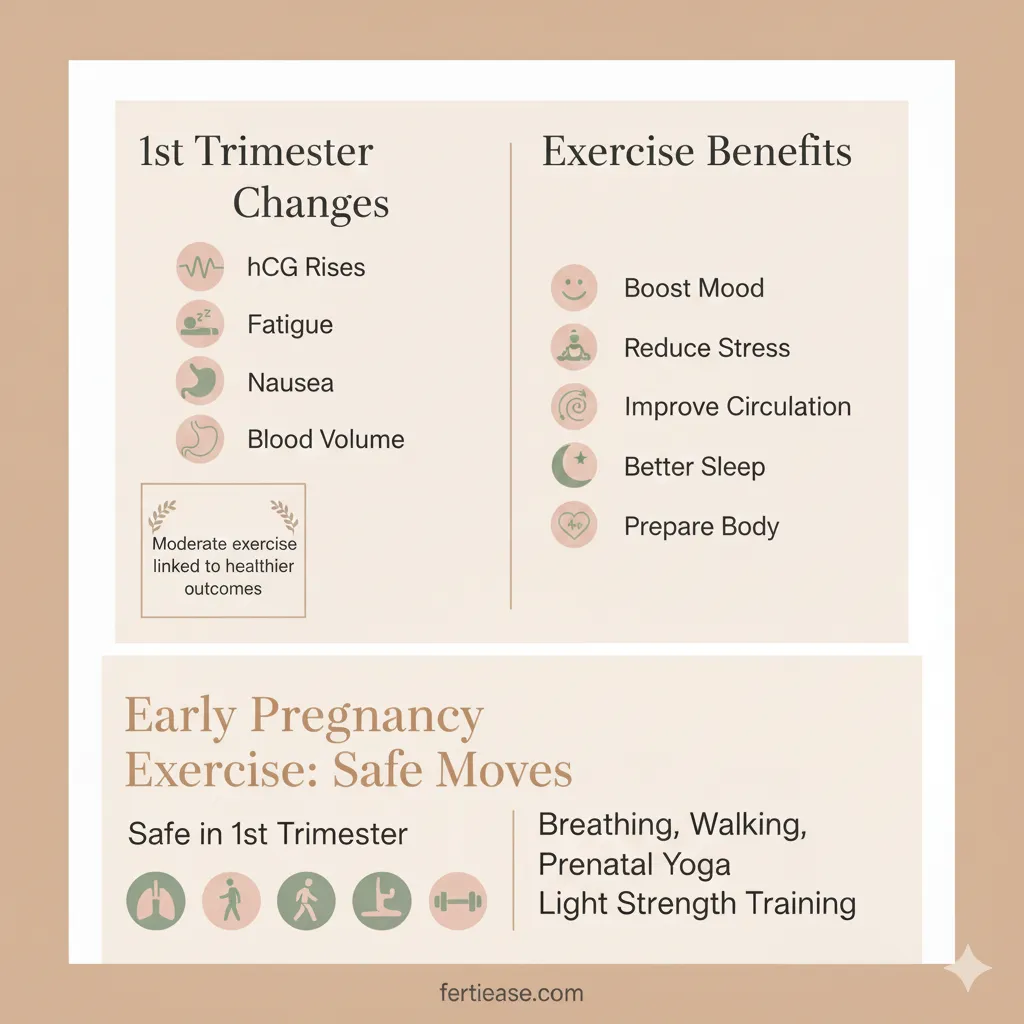
🌱 Why Early Pregnancy Exercise Matters
During the first trimester, your body undergoes dramatic hormonal changes:
hCG rises quickly
Fatigue increases
Nausea may appear
Blood volume begins to expand
Despite these changes, exercising can:
Boost mood and confidence
Reduce stress and anxiety
Improve circulation
Support better sleep
Help maintain healthy weight gain
Prepare your body for later pregnancy
In fact, research shows that moderate exercise during early pregnancy is linked to healthier outcomes, not increased risk.
🔗 External reference:
https://www.acog.org
Early Pregnancy Exercise Whats Safe In The First 12 Weeks 9 Powerful Tips 4 Fertiease
⚠️ First Trimester Reality Check
Even though exercise is generally safe, early pregnancy can feel unpredictable.
Common sensations include:
Feeling more tired than usual
Nausea during mornings—or all day
Sudden emotional shifts
Heightened sensitivity to smells
These changes mean your workout routine needs flexibility, not intensity.
Remember: consistency beats perfection.

Early Pregnancy Exercise Whats Safe In The First 12 Weeks 9 Powerful Tips 5 Fertiease
🤰 What’s Safe in Early Pregnancy Exercise?
Safe & Beneficial Activities
Walking — improves mood & circulation
Prenatal yoga — reduces stress, supports breathing
Light strength training — maintains muscle & posture
Swimming — weightless movement feels great
Prenatal Pilates (modified) — supports deep core muscles
Low-impact cycling (stationary) — cardio without impact
Breathing exercises — core & pelvic floor coordination
Each of these activities supports your changing body without overloading it.

Early Pregnancy Exercise Whats Safe In The First 12 Weeks 9 Powerful Tips 6 Fertiease
❌ What’s NOT Safe in Early Pregnancy Exercise?
Avoid or Modify:
Contact sports (risk of collision)
High-fall-risk activities (skiing, horseback riding)
Hot yoga or overheating environments
Heavy lifting with breath-holding
Exercises causing abdominal doming or bulging
Jumping or plyometrics (especially if uncomfortable)
What’s unsafe isn’t the movement itself, but the pressure, intensity, or risk involved.
📌 Related read:
👉 [Can Exercise Cause Miscarriage? 7 Powerful Facts Every Pregnant Woman Should Know]
💛 The Most Important Rule: Listen to Your Body
If you feel:
Dizziness
Nausea increases suddenly
Pelvic heaviness
Cramping that worries you
👉 Stop, hydrate, and rest.
Your body communicates more during pregnancy—trust those signals.

Early Pregnancy Exercise Whats Safe In The First 12 Weeks 9 Powerful Tips 3 Fertiease
💪 Early Pregnancy Exercise: 9 Powerful Tips for the First 12 Weeks
1. Prioritize Breathing First
Breath-led movement supports:
Pelvic floor
Deep core activation
Emotional calm
Start every workout with 1–2 minutes of slow diaphragmatic breathing.
2. Move in Short Sessions
Fatigue is real in the first trimester.
Try:
10 minutes morning walk
10 minutes afternoon stretch
10 minutes evening yoga
Movement “snacks” keep you consistent without exhaustion.
3. Keep Intensity Moderate
Use the talk test:
If you can talk while moving → safe
If you’re gasping and can’t speak → too intense
Sustainable beats intense.
4. Use Hydration Strategically
Pregnancy increases fluid needs.
Sip throughout the day—don’t chug only before workouts.
Hydration supports energy, digestion, and temperature regulation.
5. Don’t Train to “Burn Calories”
Your body is creating a human—this is not the time for weight-loss goals.
Movement now supports:
Circulation
Hormone balance
Mental health
Posture & core stability
Reframe exercise: you’re training for birth & recovery.
6. Avoid Breath Holding
This increases abdominal pressure and stresses the pelvic floor.
Instead:
Exhale during effort
Move slowly with intention
This keeps pressure gentle and supportive.
7. Track Energy Instead of Numbers
Let your energy level guide your intensity.
If the day feels heavy:
Stretching + breathing counts as exercise
If you feel strong:
Add short walks or light strength moves
No guilt, just awareness.
8. Protect Your Core Early
Abdominal doming during exercise is a clear warning sign.
If doming appears:
Reduce intensity
Modify position
Slow down movement
📌 Related read:
👉 [Pregnancy Core Workouts: What’s Safe & What’s Not]
9. Rest Without Guilt
Fatigue is your body’s request for energy conservation.
Rest is part of fitness, not a failure.
The first trimester is about adaptation, not peak performance.
🌼 Early Pregnancy Exercise by Trimester Progression
| Trimester | Exercise Focus | How It Feels |
|---|---|---|
| Weeks 1–12 | Breathing, gentle activation, mobility | Tired but adaptable |
| Weeks 13–27 | Strength & stability | Energy often returns |
| Weeks 28–40 | Comfort, posture, labor prep | Slow & supported |
Early skills support later stages.
🧬 When to Stop and Get Medical Guidance
Seek support if you notice:
Severe abdominal pain
Heavy bleeding
Sudden dizziness or fainting
Persistent shortness of breath
Fluid leakage
These symptoms don’t mean exercise caused a problem, but they signal the need for medical evaluation.
🔗 External references:
https://www.nhs.uk
https://www.acog.org
📌 Internal Links for Cluster Support
👉 [Diastasis Recti During Pregnancy: 9 Critical Things You Must Avoid]
👉 [Pelvic Floor Exercises During Pregnancy: 9 Powerful Moves for a Strong & Supported Body]
👉 [Safe Core Exercises During Pregnancy: 8 Powerful Moves to Protect Your Body]
✅ Final Thoughts
Early pregnancy exercise isn’t about intensity—it’s about connection, stability, and awareness.
Your body is already working overtime; movement should support, not stress.
If you listen to your body, move with your breath, and stay consistent—not perfect—you’ll build a foundation that supports your pregnancy, labor, and postpartum recovery.
Strong doesn’t always look like sweat.
Sometimes, strong is simply showing up gently and consistently.
What is your reaction to this article?
Here is a professional English bio for Dr. Elizabeth Williams, Obstetrician-Gynecologist: Dr. Elizabeth Williams, MD, FACOG, is a board-certified obstetrician-gynecologist with over 15 years of experience providing compassionate, evidence-based women’s healthcare. She earned her medical degree from Johns Hopkins University School of Medicine and completed her residency in Obstetrics and Gynecology at Massachusetts General Hospital, Harvard Medical School, where she served as Chief Resident. Dr. Williams specializes in high-risk pregnancies, minimally invasive gynecologic surgery, adolescent gynecology, and menopause management. Known for her warm bedside manner and clear communication, she is dedicated to empowering her patients through every stage of life, from prenatal care and childbirth to preventive wellness and complex gynecologic conditions. In addition to her clinical practice, Dr. Williams is actively involved in medical education and has published research on preeclampsia, labor induction, and robotic-assisted surgery. She is a Fellow of the American College of Obstetricians and Gynecologists (FACOG) and a member of the Society for Maternal-Fetal Medicine. Patients describe Dr. Williams as “attentive, knowledgeable, and truly caring,” and she is proud to deliver hundreds of babies each year while building long-term relationships with the families she serves. Dr. Williams practices in [City/State] and is affiliated with [Hospital Name]. She welcomes new patients and offers both in-person and telemedicine appointments.
VIEW AUTHOR PROFILE