- 1. 1. Hormonal Imbalances
- 1.1. • Thyroid Disorders
- 1.2. • Elevated Prolactin
- 1.3. • PCOS (Polycystic Ovary Syndrome)
- 2. 2. Stress and Lifestyle Factors
- 2.1. • Psychological Stress
- 2.2. • Extreme Exercise
- 2.3. • Weight Fluctuations
- 3. 3. Contraceptives and Medications
- 4. 4. Perimenopause
- 5. 5. Underlying Medical Conditions
- 5.1. • Uterine Fibroids or Polyps
- 5.2. • Eating Disorders
- 5.3. • Diabetes and Insulin Resistance
- 6. 6. When You Should See a Healthcare Professional
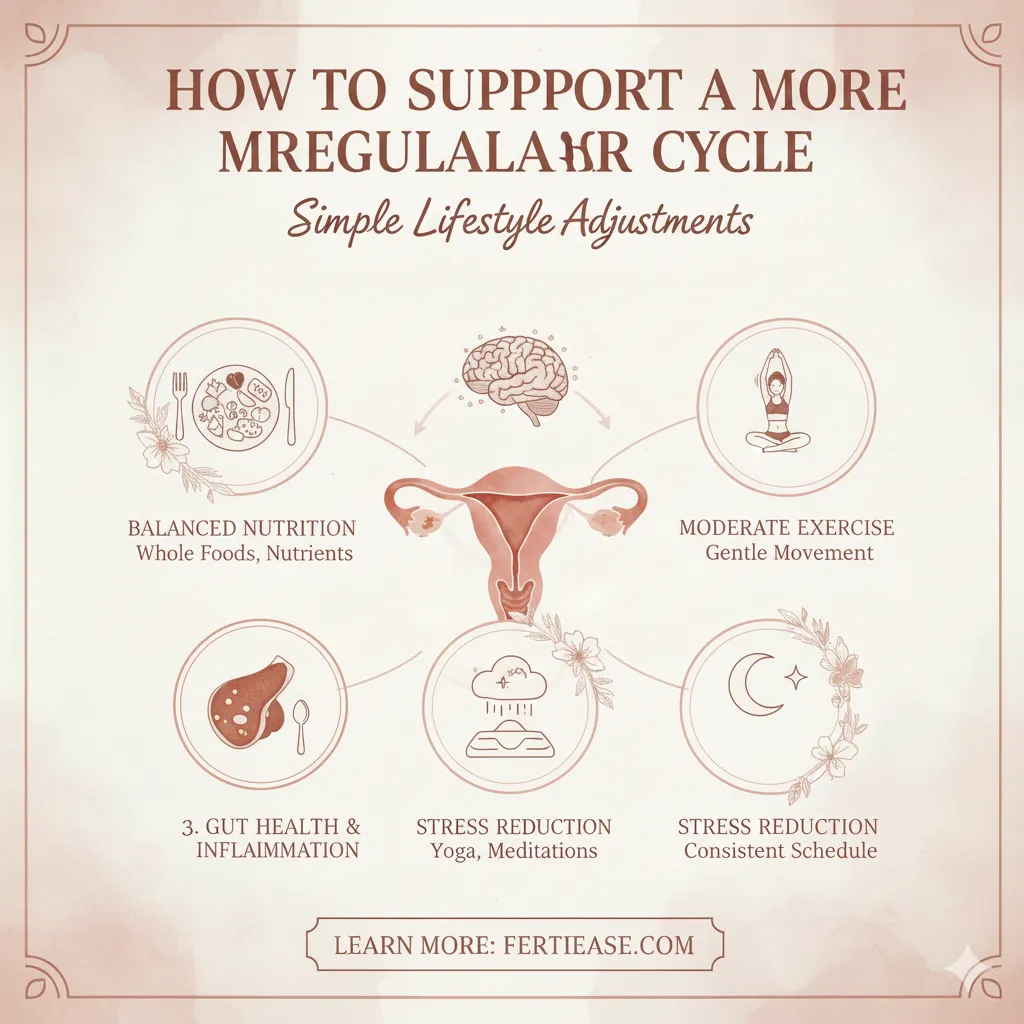
- 7. 7. How to Support a More Regular Cycle
- 8. 📣 Expert Insight
Irregular periods are one of the most common concerns among women of reproductive age. While an occasional late or early period is normal, consistent irregularity can be a sign that your body is signaling an underlying issue. Understanding the root causes behind menstrual irregularity is not only important for overall wellness—but also essential for individuals trying to conceive.
Below, we explore the most common causes of irregular cycles, supported by guidance from reputable health organizations and clinical experts.

1. Hormonal Imbalances
Your menstrual cycle is regulated primarily by the hormones estrogen and progesterone. Even slight fluctuations can shift the timing of ovulation and menstruation.
The most well-known hormonal causes include:
• Thyroid Disorders
Both hypothyroidism (low thyroid function) and hyperthyroidism (overactive thyroid) can disrupt cycle regularity.
According to the U.S. National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), thyroid hormones play a direct role in regulating the menstrual cycle and fertility.
• Elevated Prolactin
High prolactin levels, often caused by stress or a benign pituitary tumor, may delay ovulation or stop periods altogether.
• PCOS (Polycystic Ovary Syndrome)
One of the most common hormonal disorders among women, PCOS affects hormone balance, ovulation, and cycle length. The Office on Women’s Health (OWH) notes that women with PCOS may experience cycles that are longer than 35 days—or may skip cycles entirely.
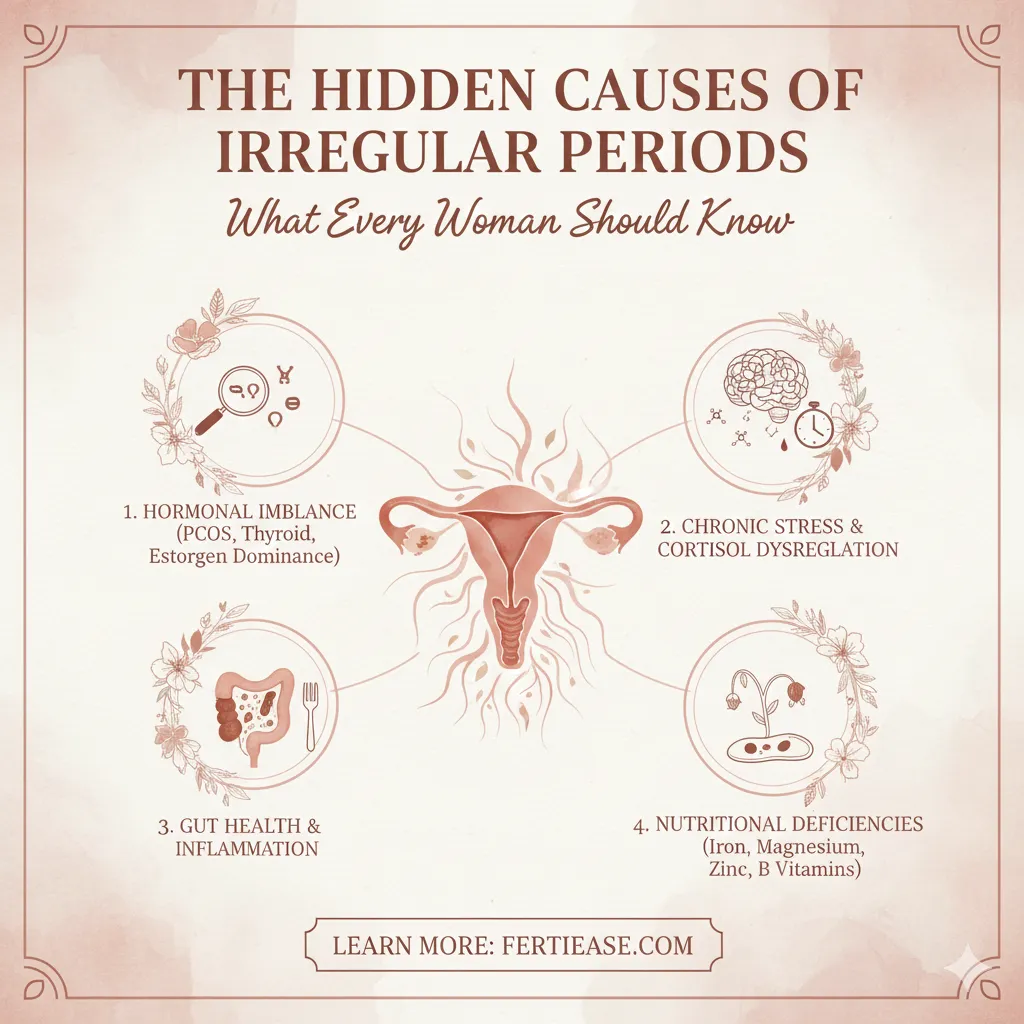
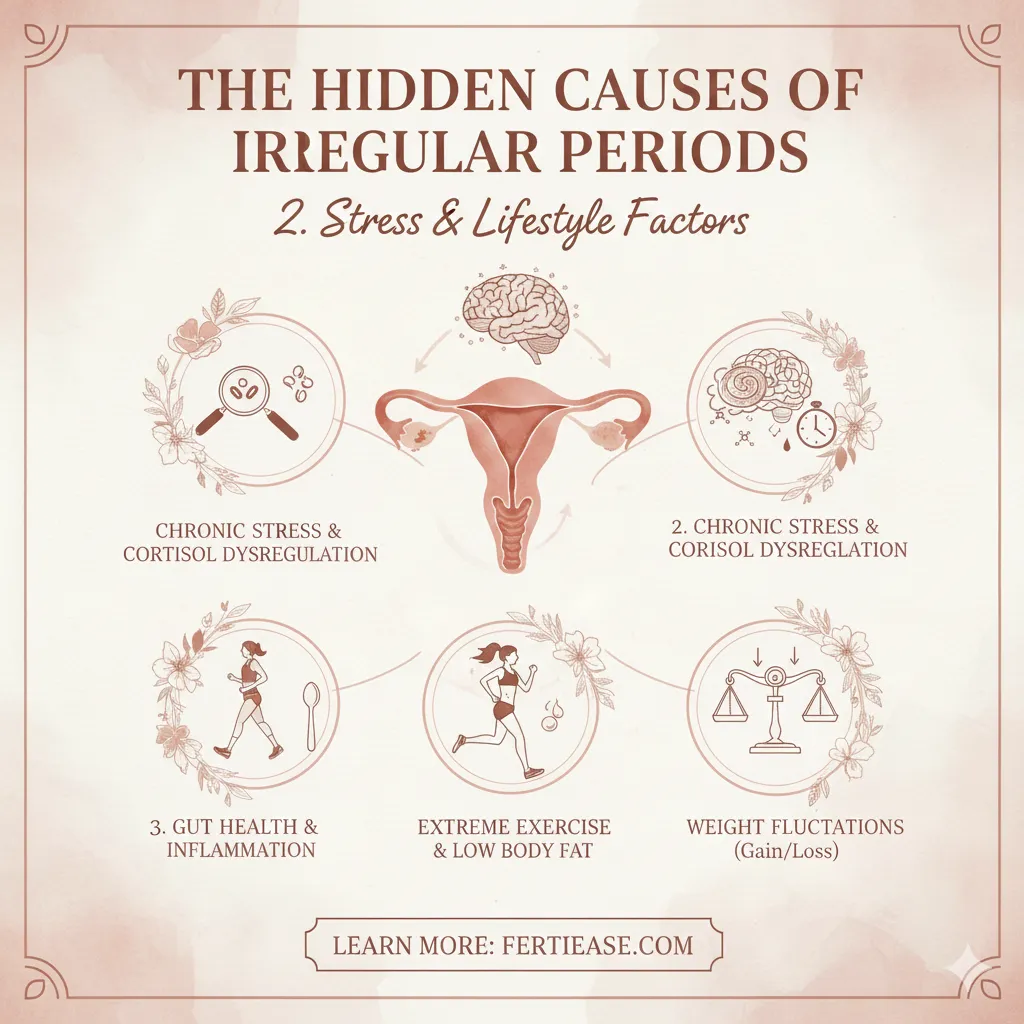
2. Stress and Lifestyle Factors
Modern life places heavy physical and emotional demands on women, and chronic stress is a well-documented trigger for cycle disruption.
• Psychological Stress
Stress impacts the hypothalamus—the brain’s “cycle control center.” When the hypothalamus senses high stress, it may reduce or suppress the hormones needed for ovulation.
Harvard Health Publishing highlights that stress-related irregular cycles are one of the most common non-medical causes.
• Extreme Exercise
Intense training or over-exercise can lower body fat percentage and hormones like leptin, both of which are required for menstrual stability.
• Weight Fluctuations
Rapid weight gain or loss affects estrogen levels. Both underweight and overweight individuals can experience delayed or absent periods.
3. Contraceptives and Medications
Hormonal birth control can temporarily change the menstrual pattern. After stopping birth control pills, patches, or injections, cycles may take several months to normalize.
Certain medications—including steroids, thyroid medications, and antipsychotics—may also affect cycle consistency.
4. Perimenopause
Women typically begin the transition to menopause between ages 40 and 50. During this stage, ovulation becomes less predictable due to fluctuating estrogen levels.
The Centers for Disease Control and Prevention (CDC) states that irregular cycles are a hallmark of perimenopause.
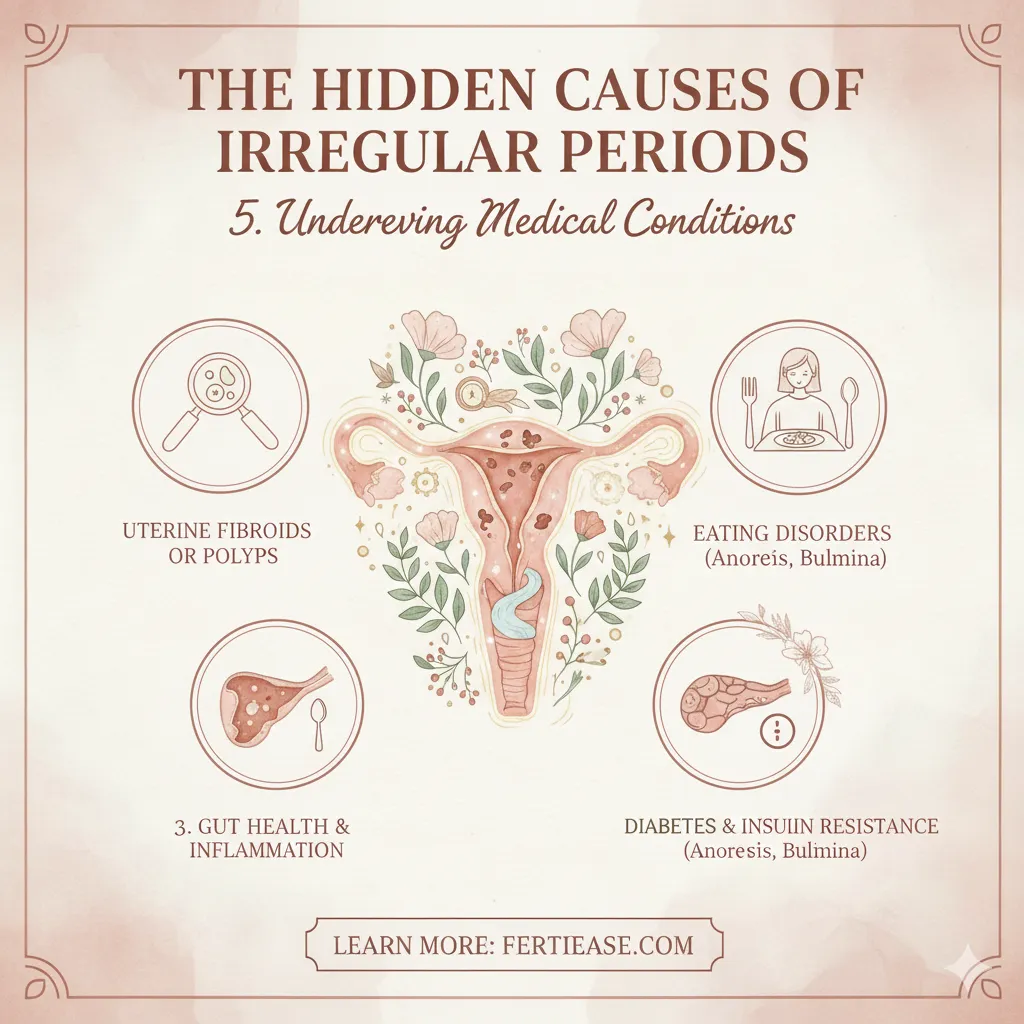
5. Underlying Medical Conditions
While many causes are benign, persistent irregular periods may indicate a deeper medical issue.
• Uterine Fibroids or Polyps
These growths can lead to heavy or irregular bleeding.
• Eating Disorders
Conditions like anorexia or bulimia can severely impact hormone production and menstrual function.
• Diabetes and Insulin Resistance
Experts at the National Institutes of Health (NIH) note that insulin resistance, commonly seen in type 2 diabetes and PCOS, can influence ovulation and cycle length.
6. When You Should See a Healthcare Professional
You should consult a doctor if:
Your periods consistently occur less than every 21 days or more than every 35 days
You go three months without a period
You experience unusually heavy bleeding
You’re trying to conceive and your cycles are unpredictable
Early evaluation helps address underlying issues before they affect fertility or overall health.
7. How to Support a More Regular Cycle
While medical conditions require professional care, some lifestyle adjustments can help:
Maintain balanced nutrition
Aim for moderate, not excessive, exercise
Practice stress-reducing activities like yoga or meditation
Track your cycle using a fertility app
Ensure adequate sleep
These habits help support hormonal balance and cycle health over time.
📣 Expert Insight
Dr. Karen Carlson, a board-certified obstetrician-gynecologist, emphasizes:
“A woman’s menstrual cycle is one of the clearest indicators of her health. Persistent irregularity should not be ignored. Identifying the underlying cause early allows for better treatment outcomes and can significantly improve fertility prospects.”
What is your reaction to this article?
Hi, I’m Mary! I’m a women’s health educator, certified Fertility Awareness Method (FAM) instructor, and a total cycle nerd who’s been charting my own cycles for over a decade. After ditching hormonal birth control in my mid-20s and realizing how little I actually knew about my body, I dove head-first into the science of natural fertility tracking. What started as a personal experiment turned into a full-on passion: helping women reclaim their cycles, conceive confidently, or avoid pregnancy without side effects. When I’m not geeking out over cervical mucus patterns or BBT charts, you’ll find me sipping herbal tea, tending my (slightly chaotic) houseplant jungle, or walking my rescue dog with a podcast in my ears. I believe knowledge is power, and understanding your cycle is one of the kindest things you can do for yourself. Thanks for being here — let’s decode your body together! 🌿
VIEW AUTHOR PROFILE